- Conditions
- Procedures
- Patient care
- Why choose us
- Our Doctors
- Contact
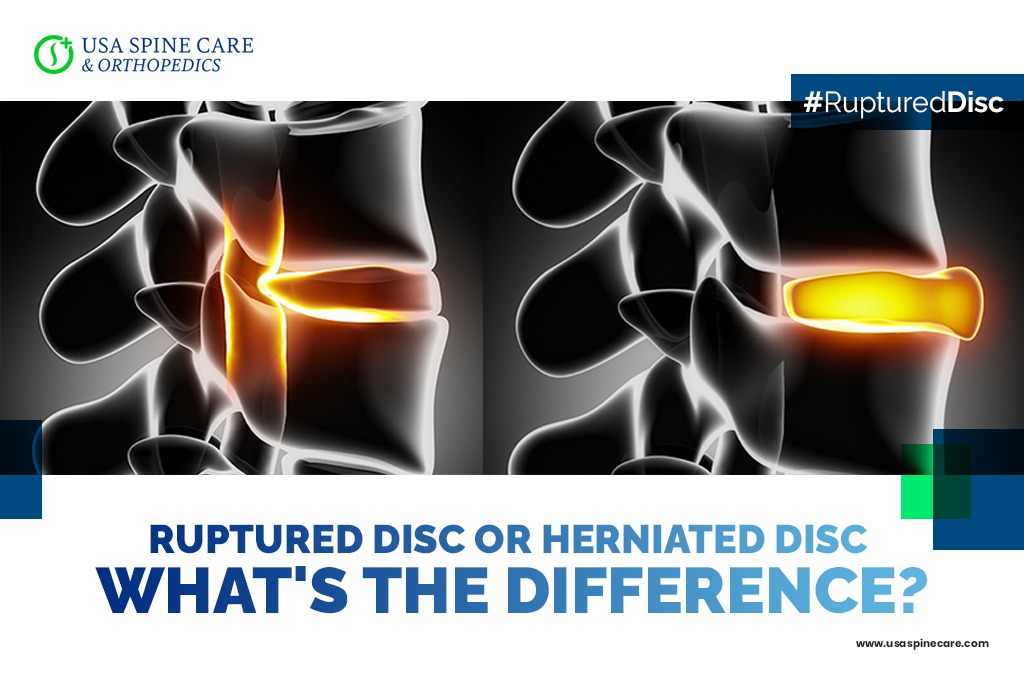
Ruptured Disc or Herniated Disc | What's the Difference?
There are a large number of terms that doctors, chiropractors, other medical professionals and patients use to describe conditions and injuries that affect the spinal discs. Although bulging and herniated discs are two of the most common conditions people encounter, another diagnosis is a ruptured disc. While this can be an alarming condition to find out that you have, it is generally not a medical emergency — although it can be a source of severe and debilitating pain.
Because the term ruptured disc and herniated disc are sometimes used interchangeably, many patients ask what the difference between the two conditions are. To help you understand the difference between ruptured and herniated discs, and how that may affect treatment for neck and back pain, we’re happy to provide the following information.
If you’d like to learn more or you need answers to any other questions you have, we invite you to contact a member of our caring team today.
The difference between a ruptured disc and a herniated disc
Doctors and other medical professionals such as a radiologist or chiropractor will often consider a ruptured disc as a specific type of herniated disc. A herniated disc occurs when inner disc material, known as the nucleus, pushes out through a tear or weak spot in the tougher outer layer. A rupture may be described when there is a full tear in the outer layer and nucleus material is exposed and pushes out into the spinal column.
There are different methods of classification for disc conditions among medical professionals, so it is possible to hear a different usage for this term, even from physicians. However, what the two terms definitely have in common is that they can cause spinal narrowing and nerve compression that results in severe neck and back pain as well as other symptoms.
Ruptured disc and herniated disc causes and risk factors
Like a herniated disc, a ruptured disc is primarily an age-related degenerative condition. The spinal discs play an important role as shock absorbers in the spinal column. With a disc between nearly every vertebra, they separate and cushion the spine, allowing us to bend and flex.
As we age, the discs begin to dry out and lose elasticity, making them less able to withstand the tremendous amount of stress they are put under on a daily basis. This leads to the formation of small cracks and tears in the outer layer, which can grow over time. As the discs are put under pressure during our everyday movements, the inner nucleus can push out through these tears, resulting in a ruptured disc.
A ruptured disc or herniated disc is necessarily a painful condition by itself. However, if the ruptured disc material narrows the already tight space in the spinal column, it can result in painful compression or irritation of the spinal nerves. This can result in neck pain, back pain, and radiating symptoms such as tingling and numbness that can have a negative impact on your activity level and quality of life.
A ruptured disc can often improve through conservative therapies
Upon diagnosis of a ruptured disc, herniated disc or any other condition causing painful symptoms, a doctor or chiropractor will usually recommend starting with conservative treatment. This can include:
- Rest
- Hot and/or cold therapy, such as a heating pad or ice pack
- Physical therapy
- Manual adjustment
- Massage therapy
- Pain-relieving steroid injections
The goal is to improve symptoms and function while the progress of the condition is monitored. In some cases, a ruptured disc can improve on its own, and many patients are able to experience long-term relief from neck and back pain without the need for surgery.
When to consider surgery for a ruptured disc
Surgery for a ruptured disc can become a serious consideration if conservative therapies have been fully explored without finding the relief necessary for a good quality of life. Surgery can include decompression procedures, such as a discectomy, which involves only removing the disc material that is causing nerve compression. For more severely damaged discs, the surgeon may need to remove the full disc and perform a stabilization or fusion procedure to stabilize the spine.
In many cases, surgeons are able to perform these procedures on an outpatient basis through a muscle-sparing, minimally invasive approach.
Reach out to the caring and dedicated USA Spine Care team today
To learn more about your options for relief if you’ve been diagnosed with a ruptured disc, contact USA Spine Care today. We specialize in conditions that cause neck and back pain and can help you develop a personalized treatment plan no matter where you are on your journey to relief.
Call 1-813-773-3050
Ruptured Disc Quick Answers
How serious is a ruptured disc?
A ruptured disc is not typically seen as a medical emergency, but it can be a significant source of pain and mobility problems. This means that patients should take diagnosis and treatment to find lasting relief and improved quality of life. However, in rare cases, ruptured discs can cause a potentially life-threatening condition known as cauda equina syndrome. If you experience loss of sensation and movement in the lower body or bowel and/or bladder incontinence, it is critical to seek immediate medical attention.
Can a ruptured disc heal on its own?
It is possible for an individual instance of a ruptured disc to heal with time and proper treatment, particularly in younger patients. Since a ruptured disc is an age-related degenerative condition, it becomes harder for the discs to heal as we get older and more likely for the condition to develop. For many people, the primary goal of treatment is to manage symptoms, improve function and promote overall health and spine health.
Is it possible to repair a ruptured disc?
A ruptured disc that does not respond to conservative therapies may be treated with a surgical decompression procedure known as a discectomy. The goal of a discectomy is to access the spine and remove ruptured disc material that is causing compression and/or irritation of nerves in the spinal column. This procedure can often be performed on an outpatient basis with the help of minimally invasive techniques.
What is the difference between a herniated disc and a ruptured disc?
These terms are often used interchangeably, including by many medical professionals. Doctors and radiologists may classify ruptured discs as a more severe type of herniated disc where the inner disc material fully extends out through a crack or tear in the outer layer.
