- Conditions
- Procedures
- Patient care
- Why choose us
- Our Doctors
- Contact
Home » Spine Conditions »
Everything you need to know about a prolapsed disc
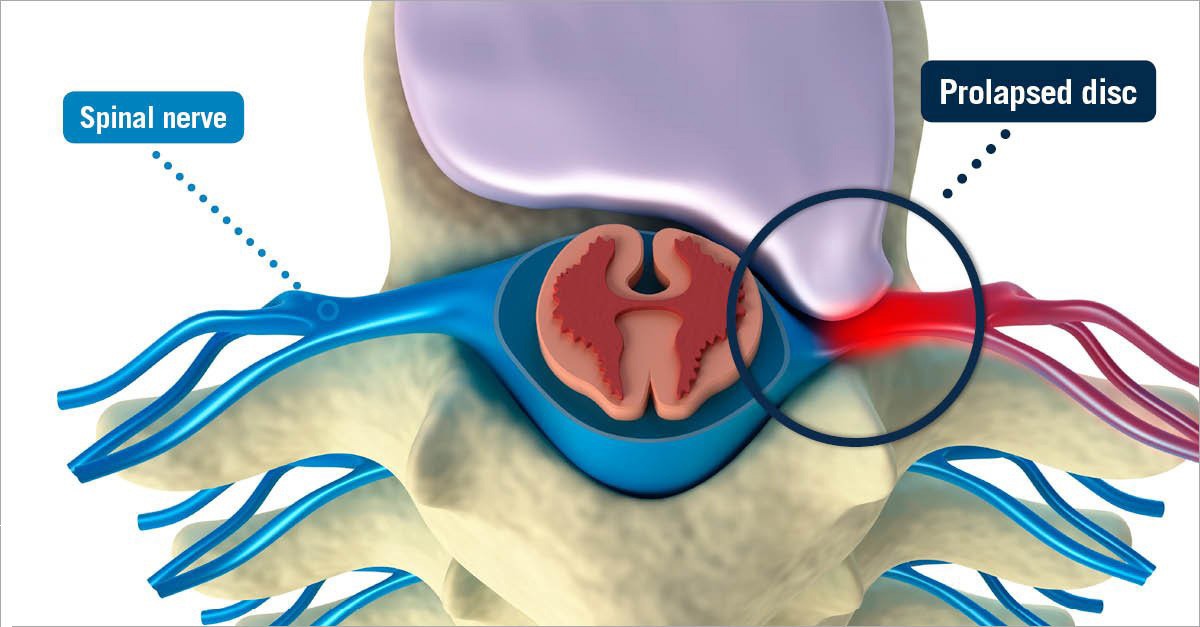
A prolapsed disc is a condition that is commonly referred to in several different ways, including a ruptured disc, a herniated disc and a slipped disc. All of these terms are used interchangeably to indicate that a portion of a disc’s gel-like nuclear material has leaked out into the spinal canal through a tear or split in the disc’s layered, cartilaginous outer wall. This condition can occur at any level of the spine, but it is most frequently found in the lower back, where the lumbar vertebrae and discs bear much of the body’s weight, and where the body’s ongoing movements produce significant stress on the spine over time.
Disc degeneration often occurs in several stages, and disc prolapse takes place at a relatively early stage. When a disc becomes thinner, drier or weaker due to age or injury, it can begin to protrude beyond its normal position between the vertebrae. This condition can eventually lead to a full herniation, or tearing, of the disc’s outer wall and the subsequent extrusion of nuclear material.
If you think you have a prolapsed disc or other disc damage — such as a disc herniation — in your spine, you should contact your doctor to receive a proper diagnosis and discuss the possible treatment options. Your doctor can answer any questions you have and help you take a step toward pain relief.
Causes of a prolapsed disc
A traumatic spine injury can cause a prolapsed disc, but the condition is most often related to the normal wear and tear that occurs over time on the parts of the spine. While cumulative stress on the spine is inevitable, certain factors have been shown to increase the likelihood that an individual will develop a prolapsed disc, such as heredity, repetitive activity, prolonged inactivity, an unhealthy weight and smoking.
As part of the natural aging process, the water content within the discs slowly begins to diminish. When a disc becomes dehydrated, it loses flexibility and becomes brittle, and is less able to withstand the normal pressures being exerted by the vertebrae situated immediately above and below it. As a result, a chain reaction can occur in which the gel-like inner material (nucleus pulposus) of the compromised disc exerts pressure on the tough, fibrous outer wall (annulus fibrosus) that normally contains it. As pressure builds on the already weakened disc wall, its integrity can be compromised. A tear can begin to form — typically starting on the inside of the disc and working its way outward — and the inner-disc material can begin to force its way out through the opening, leading to a prolapsed disc.
Symptoms of a prolapsed disc
In many cases, a prolapsed disc is asymptomatic and remains undetected, allowing you to go about your daily life as usual. However, if the extruded disc material irritates nerve endings in the disc’s wall or impinges an adjacent nerve root or the spinal cord itself, it can produce uncomfortable symptoms like localized discomfort and radiating pain, tingling, numbness, stiffness and muscle weakness.
The symptoms that arise when extruded disc material irritates or compresses sensitive neural tissue can manifest either locally or elsewhere in the body, depending on the area of the body affected by the compressed nerve root. There are 31 pairs of nerve roots situated along the spine — which spans from the neck to the coccyx (tailbone) — including eight in the cervical region, 12 in the thoracic region, five in the lumbar region, five in the sacrum and one in the coccyx.
A prolapsed disc in the cervical region
The nerve roots in the cervical spine send signals to the head, diaphragm, upper body, arms, wrists and hands. Therefore, a prolapsed disc in the cervical region can produce migraine headaches and other symptoms that affect the:
- Neck
- Shoulders
- Upper back
- Deltoids
- Triceps
- Biceps
- Forearms
- Wrists
- Hands
- Fingers
A prolapsed disc in the thoracic region
The nerve roots in the thoracic spine send signals to the upper back, chest, torso and ribs. Because the thoracic vertebrae are relatively rigid, the discs in between those vertebrae are less susceptible to prolapse than those discs cushioning the more flexible vertebrae located in the cervical and lumbar regions. Nevertheless, when a thoracic disc prolapse occurs, it can produce symptoms that are very similar to the signs of other serious conditions, such as those affecting the heart, lungs, kidneys and gastrointestinal system. Therefore, a prompt and accurate diagnosis of the root cause of any form of chest pain, balance loss or abdominal discomfort is imperative.
A prolapsed disc in the lumbar region
The nerve roots in the lumbar spine travel to the lower back, hips, buttocks, legs, ankles, feet and toes. The highly flexible vertebrae in the lower back make the discs between them especially vulnerable to degeneration and disc prolapse. A prolapsed disc in the lumbar region that presses on spinal nerves can produce symptoms that affect the:
• Low back
• Hips
• Buttocks
• Legs
• Ankles
• Feet
• Toes
Prolapsed disc treatments
The type of prolapsed disc treatment prescribed by a physician will depend on the severity and location of the damaged disc. Most patients find that disc prolapse symptoms can be treated conservatively with activity modification, physical therapy, pain and anti-inflammatory medications, stretching, low-impact exercise and/or a limited period of rest. Additionally, some patients find alternative treatments like acupuncture, chiropractic therapy and massage to be highly effective as well.
For pain that is severe or debilitating, a physician might recommend a series of corticosteroid injections, which can reduce painful inflammation to produce relief that lasts for weeks or months. Surgery, while viable for some patients, is usually considered to be a last resort for treating a prolapsed disc, and surgical intervention is typically advised only after several weeks or months of conservative therapy prove to be ineffective for helping you to find symptom relief and achieve a better quality of life.
Surgery for a prolapsed disc
If severe neck or back pain persists after several weeks or months of conservative prolapsed disc treatment, USA Spine Care might be able to help. Our skilled surgeons have perfected advanced techniques that they use to perform minimally invasive, outpatient procedures, which can help patients find relief from the pain associated with a prolapsed disc.
As opposed to simply managing symptoms, the goal of prolapsed disc surgery is to address their underlying cause by removing the disc material that is exerting painful pressure on the pinched nerve in the spinal column. To treat this condition, the minimally invasive spine surgery available at USA Spine Care is often the clinically appropriate first choice. Our advanced procedures offer patients many advantages over traditional open back surgery. Contact us to learn more or request a no-cost review of your recent MRI scan* to find out if you are a candidate for minimally invasive spine surgery.
